Biotronix Un Weight Mobility Trainer /Partial Body Weight Support System/Suspended Gait Trainer Dual Function Motorized ( Wheel chair to Standing ( Vertical Oscillation) ,Standing to Lifting ) Deluxe Model ( Without Treadmill )
Product Specification
| Brand | Biotronix |
| Usage/Application | Gait Training |
| Material | Mild Steel and Stainless Steel |
| Type | Exercise Equipment |
| Un-Weigh Mobility Trainer/Gait Trainer with battery back-up. | |
| HEIGHT ADJUSTABLE | YES. |
| BATTERY BACK UP | YES. |
| LOAD MONITOR | DIGITAL DISPLAY. |
| MOUNTED ON | LOCKABLE WHEELS. |
| HANDRAIL | PROVIDED Stainless Steel |
| HARNESS | ADULT AND CHILD |
| Minimum Order Quantity | 1 |
Product Description
The electrical un-weighing trainer is designed to apply vertical support to remove the stress of bearing body weight; unit digitally controls weight bearing, and promotes proper posture and balance over a treadmill or the ground.
The system allows patient to stand upright and use both arms freely. Harnesses give security to patients with limited trunk strength. The adjust-table suspension bar adjusts to accommodate tall Children & Adults.
SPECIFICATIONS:
* Un-weighing: Can be set 0% to 100% of the body weight, digitally.
* Un-weighing System: Electrical, the unit comes with mains operated built in lift system.
* Vertical Oscillation: Up to 24", ideal for sit to stand exercises also.
* Suspension: Single point, with 360 degree rotational bar to help patient turn easily.
* Control Panel: Digitally display
*Weight Capacity: 0-140 kg un-weighing range.
* Un-Weighing Harness: Two, Small and Standard size.
* Handrails: For patient's support, Adjustable & Removable.
Provides proper posture, reduces weight bearing, eliminates concerns for balance, and facilitates the training of coordinated lower extremity movement.
Creates an ideal environment for treating patients with a wide range of impairments and functional levels.
Unique harness design not only permits unilateral or bilateral support allowing progression of the weight bearing load from non to full weight bearing, but also allows the clinician to manually assist the legs and pelvis to achieve proper gait patterns.
We at have provided a mobile design for easy gait therapy.
As the original partial weight bearing therapy device, has forever altered gait therapy techniques, as well as expectations of outcome.
Sit 2 Stand feature allow un-weinging of the patient at most safe environment with zero risk of fall or injury
Quality harness for Pelvic Stabilization. Available for both pediatric and adult community.
Application
- Neuro-rehab
- Orthopedics
- Paediatrics
- Stroke
- Spinal Cord
- Head Injury
- Amputees
- Neurologic
- Vestibular
- Geriatrics Patients
Specification
-
Un-weigh - Electrical cum Battery power un-weigh system
-
Load Cell Suspension - Single point with 360° rotational bar to help patients turn easily for forward & backward walking
- Digital Weight Display
-
Vertical Oscillation - Electrical / Battery powered, Adjustable vertical oscillation upto 24" helps to assemble at low height/ceilings, ideal for sit to stand exercises
-
Handle for easy mobility
-
Handrails - adjustable, removable patient handrails accommodates for easy support / treadmil access Easy to remove for specific balance training exercise
- Hand Remote - Low effort, no manual operation - un-weigh, vertical uplift, which is easily control vide one hand remote only
USER FRIENDLY DESIGN
- Supporting option of Stainless steel / Mild Steel body frame is designed in such a way that it allows therapist easy access to Patient to assist the patient in quality rehab training.
- This Device controls weight bearing posture and balance of patient over treadmill or over ground automatically.
ERGONOMIC CONTROLS WHICH ADAPT TO PATIENT NEEDS
- Compatible with support for lifting patient from seated position such as a wheel chair / Bed.
- Its internal width supports Treadmill
- Includes Hand rails are adjustable vertically for height and horizontally for closeness of hands towards inside
- Supports patient weight up to 200 Kgs
- Suitable for pediatric and adult up to 6’3” height.
Biotronix Un Weigh System is an Unweighing system which provides Unweighing support for treadmill users or as a standalone Unweighing system. This system helps patients undergo Gait training by partially supporting their weight, to provide continuous and medically safe support for patients as they walk or run on the treadmill. Therapists can use this system for rehabilitating patients diagnosed with a wide range of gait disorders stemming from ortho, neuro, strokes or spinal cord injuries. Incorporating an attached harness and support for pelvic support and vertical displacement, this system adjusts to individual patient needs and therapist specifications to curb balance problems and improve motor coordination.
- 1 pc Biotronix Un Weight Mobility Trainer /Partial Body Weight Support System/Suspended Gait Trainer Dual Function Motorized ( Wheel chair to Standing ( ( Vertical Oscillation)) ,Standing to Lifting ) Deluxe Model ( Without Treadmill )Physiotherapy and Rehabilitation Equipment
- 1 Hand Remote Control
- 1 Complementary Physio Chart Set ( 6 wall pasted physio charts )
Warranty Details : 3 Year Motor Warranty against manufacturing Defect.











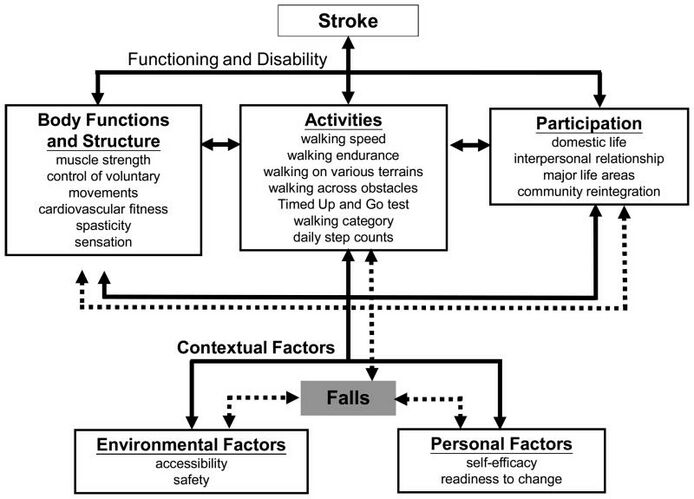
Gait Training in Stroke
Introduction
The functional limitations and impairments after a stroke are unique to each individual and often include impairments in mobility. Gait recovery is a major objective in the rehabilitation program for persons with stroke, and often a person's top goal. Restoring function after stroke is a complex process involving spontaneous recovery and the effects of therapeutic interventions. Although the majority of persons with a stroke regain the ability to walk, many do not achieve the ambulation endurance, speed, or security required to perform their daily activities independently and safely. Falls are a common concern for community-dwelling persons with stroke.
Potential limitations Observed CVA Effecting Gait
Include changes in:
- Muscle tone (spasticity or flaccidity)
- Muscle strength
- Timing of the gait cycle, resulting in an asymmetrical gait pattern
- Walking speed
- Balance systems
- Sensation
- Visual scanning
- Cognition and safety awareness
- Soft tissue length (contractures)
Stroke Rehabilitation Principles
"Normal" gait is a complex activity and skilled personalized therapeutic interventions are needed for successful stroke rehabilitation. Several general principles underpin the process of stroke rehabilitation:
- Good rehabilitation outcome seems to be strongly associated with high degree of motivation, and engagement of the patient and their family.
- Setting goals according to specific rehabilitation aims of an individual might improve the outcomes.
- Cognitive function is strongly related to successful rehabilitation. Attention is a key factor for rehabilitation in persons with stroke as poorer attention performances are associated with a more negative impact of stroke disability on daily functioning

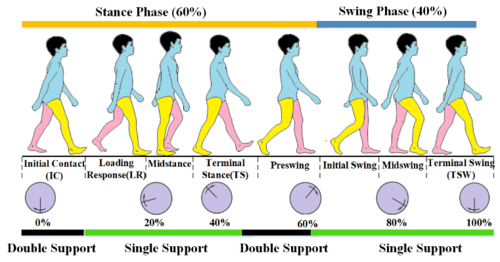
Understanding Normal Gait
Gait training, regardless of the client's diagnosis, is based on an understanding of "normal" gait. During a therapy evaluation, it is important to gather information on the person with stroke's baseline level of activity and mobility - this data can be collected from the person themselves or reliable family members or friends. All this information is taken into account when creating a person's individualized therapy program.
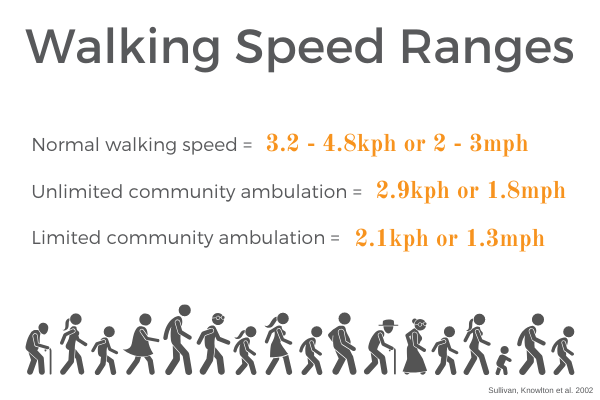
The ability to walk independently is a prerequisite for most daily activities, whether a person is homebound or a community distance ambulator. Think of all the skills needed to safely negotiate a community setting: cross a street in the time allotted by pedestrian lights, to step on and off a moving walkway, in and out of automatic doors, avoid obstacles, negotiate curbs, multi-task mobility with environmental scanning, understand the safety signals found in your environment. A walking velocity of 1.1-1.5 m/s is considered normal baseline speed to safely function as a community dwelling individual. It has been reported that only 7% of patients discharged from rehabilitation met the criteria for community walking, which included the ability to walk 500 m continuously at a speed that would enable them to cross a road safely
The major requirements for successful walking include:
- Support of body mass by lower limbs
- Propulsion of the body in the intended direction
- The production of a basic locomotor rhythm
- Dynamic balance control of the moving body
- Flexibility, i.e. the ability to adapt the movement to changing environmental demands and goals.

Gait after Stroke
Abnormal gait patterns are a common impairment following a stroke due to disruption of neural pathways in the motor cortex, their communication with the brainstem and its descending pathways and intraspinal locomotor network. This damage results in observed muscle weakness, changes in muscle tone, and abnormal synergistic movement patterns commonly seen in persons with stroke.. Secondary impairments stemming from the cardiovascular and musculoskeletal systems stemming from disuse and physical inactivity can add to ambulation difficulty. The resulting gait pattern following stroke is often a combination of movement deviations and new compensatory movement patterns, unique to that person's injury. As with all rehabilitation programs, gait training with a person following a stroke is highly individualized. The below video shows an example of progressive intensive individualized gait training.
Gait Training
Therapeutic Interventions
Stroke rehabilitation is highly individualized to a person with stroke's needs. A physical therapy plan of care can include any or all of the following interventions to improve ambulation ability:
- Preventing adaptive changes in lower limb soft tissues
- Eliciting voluntary activation in key muscle groups in lower limbs
- Increasing muscle strength and coordination
- Increasing walking velocity and endurance
- Maximizing skill, eg increasing flexibility
- Increasing static and dynamic balance
- Increasing cardiovascular fitness
- Increasing safety awareness
- Education on proper use of assistive devices

Conventional Gait Training
Conventional gait training (over ground gait training) involves breaking down parts of the gait cycle, training and improving the abnormal parts, then reintegrating them into ambulation to return to a more normal gait cycle. This can include the following:
- Symmetrical weight bearing between lower limbs in stance
- Weight shifting between lower limbs
- Stepping training (swinging/clearance) over level and unloved surfaces
- Heel strike/limb loading acceptance
- Single leg stance with stable balance and control
- Push off/initial swing of moving leg
The following components of gait are key to successful ambulation:
- Support of the center of gravity (COG) by the lower limbs
- Propulsion of the COG by the lower limbs
- Balance of the COG as it transitions between weight bearing limbs
- Controlling knee and toe paths for toe clearance and foot placement
- Optimizing rhythm and coordination.
Observe for abnormalities of any of these parts and develop therapeutic interventions to improve those skills. It is important to gather information on a person's normal environment during your evaluation and continued assessment. This information will help shape your gait training plan of care to include skill such as:
- stair and curb negotiation
- ambulation over obstacles
- ambulation over carpet, tile, doorway thresholds
- ambulation over changes in grades such as ramps and slopes
- ambulation over uneven outdoor surfaces such as grass, loose rock, wet surfaces, sidewalks, road surfaces
Special consideration for persons with stroke during gait training is the potential need for orthotics to assist with abnormalities such as drop foot. Read more about orthotics.
Strength Training
All rehabilitation programs will involve strength training. This can be performed as a formal exercise program or through functional activities.
- Circuit training
- Strength training to improve walking ability
- Task-specific training to improve walking ability

Neuromuscular Reeducation (NMR)
Neurofacilitation techniques to inhibit excessive tone, stimulate muscle activity (if hypotonia is present) and to facilitate normal movement patterns through hands-on techniques.[9] Practice based on the framework advocated by Berta Bobath remains the predominant physical therapy approach to stroke patients in the UK and is also common in many other parts of the world, including Canada, United States, Europe, Australia, Hong Kong and Taiwan. It has evolved from its original foundations, however elements still emphasize normal tone and the necessity of normal movement patterns to perform functional tasks [10] Examples of NMR handling techniques include:
- Neuro Developmental Technique (NDT)
- Kinesio taping
- Neuro-IFRAH
Body Weight Supported Treadmill Training
Body Weigh Supported Treadmill Training (BWSTT) involves the use of a suspension system with harness over a treadmill for gait training. The person with stroke is secured in the harness for fall prevention, then is positioned over the treadmill and attached to the suspension system. Gait training with this modality allows for more control over the ambulation environment (level surfaces, grade of surface), control over the speed of ambulation, and allows one or more therapists to provide tactile cues or physical assist to achieve gait dynamics. The person can be unweighted by the suspension system, this reduces the amount of weight bearing through their lower limbs and gives the feeling of being lighter. Ambulation will therefore require less effort by the person during initial gait training sessions. Body weight can be slowly added back to the person's control as they progress through their BWSTT program. Skilled therapists can assist with limb advancement, heel strike, stance with knee control, and swing phases of gait with tactile cues. Upright posture can also be addressed with this treatment modality. The video below demonstrates how to setup a BSW treadmill system, handling techniques, and how to advance to suspension system to overground gait training.

Body Weight Supported Treadmill Training in Neurological Rehabilitation
Neurorehabilitation encompasses a wide range of medical interventions aimed at helping people recover from a nervous system injury, such as traumatic brain injury, stroke, or spinal cord injury.
The goal of neurorehabilitation is to optimize recovery, minimize compensations, and increase the intensity of skill practice¹. The human brain and body are extremely efficient at finding ways to accomplish tasks after an injury. However, even though the task gets accomplished, it might not be the best for your recovery.
For example, if someone is trying to walk after a stroke, they will often lean to their stronger side and then swing their weaker leg forward in order to take a step. This is one way of moving forward, but clearly not the most efficient way to walk.
In order to optimize recovery for a client after a neurological injury, we want to create the right environment and provide the assistance necessary to complete the task without unnecessary movements, in other words, minimize compensations.
Furthermore, it is not enough to accomplish this task once or twice, it requires a high level of repetition and challenge while practicing this skill, in order to make a positive and permanent change towards recovery.
One method used in neurorehabilitation to create a more optimal environment, to provide the appropriate assistance, and to improve a client’s postural control, is the body-weight supported treadmill. The body-weight supported treadmill training allows therapists to give their clients the necessary support when completing many different tasks such as standing, balance training, stepping, reaching and walking.

Walking: A Complex Whole Body Activity
Human locomotion combines multiple body systems and is incredibly complex. Your body unconsciously allows you to do all of the following:
- Bipedal progression of the centre of mass with dynamic equilibrium (i.e. moving your body forward and upright)
- Adapts to destabilizing factors from an anticipatory and reactive perspective (i.e. reacting to things in your way and things you didn’t anticipate)
- Utilizes coordinated synergies of upper limbs, trunk, head and lower limbs
For example, think about the last time you walked from your car to your home. During that walk you stepped out of your car, moved around your vehicle, stepped onto the sidewalk or path, climbed up several steps, and then walked through your front door and into your home.
Think about the amazing number of movements that took place without one conscious thought of how you were moving your legs, placing your steps, or adjusting for different environments.
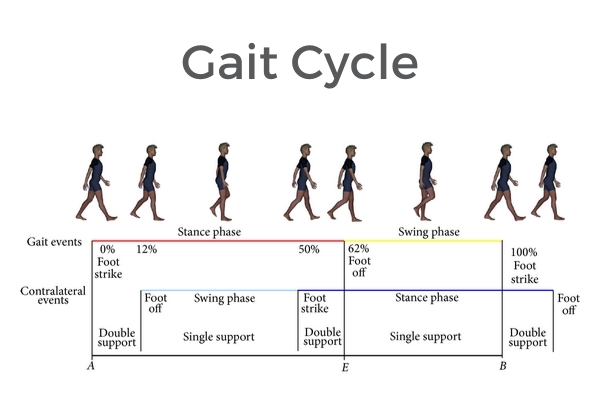
Here is a schematic representation of gait cycle with stance (red) and swing (yellow) phases showed in the above line, whereas the line drawn in middle reported the gait cycle of the contralateral limb with swing (light blue) and stance (blue) phases.
Posture and Walking
Before you even start walking, your neurological system prepares. We have three ways in which we get ready for movement.
- Early postural adjustments (-600 to -200ms before the movement) help to create adequate mechanical conditions for the expected (planned) perturbation (action)².
- Anticipatory Postural Adjustments (-200ms to 0) minimize the negative consequences of a predicted postural perturbation³.
- Anticipatory Synergy Adjustments (ASA’s) modify the stability (reproducibility) of performance variables4.
All of these anticipatory systems are influenced by body alignment, amount of practice, and velocity of the movement, which are all variables incorporated into body-weight support treadmill training.

Body weight supported treadmill training will directly increase the demand placed on the postural control mechanisms of your body and thus the production of anticipatory postural adjustments. This means that using the body-weight supported treadmill training helps to prepare your body to achieve the right alignment and posture to walk.
The Central Pattern Generator (CPG)
Once you have started walking, your neurological system has a network of neurons within your spinal cord which helps to generate rhythm and the locomotor pattern5.
Sensory information from a variety of sources within the visual, vestibular and proprioceptive systems are utilized by the CPG to keep you walking smoothly6.
Using BWSTT to Improve Walking
During body weight supported treadmill training, the client is partially suspended in a harness either from the ceiling or from an apparatus frame. This helps to reduce the client’s overall weight bearing and provides postural stability.
It also enables the integration of the client’s postural control and stepping in a safe, variable, dynamic task specific environment7 either over the ground or on a treadmill. The amount of support can be gradually decreased as postural control, balance, and coordination begin to improve.
At Propel Physiotherapy, we use the LiteGait system for body weight support in combination with a treadmill, to provide body-weight supported treadmill training for many of our clients with neurological injuries. The effects are safe, cumulative, non-invasive.

The Evidence for Body Weight Supported Treadmill Training
Body weight supported treadmill training is considered one of the newest evidence-based clinical approaches to locomotor rehabilitation, enabling task-specific training, thereby inducing activity-dependent neuroplasticity8. A recent Cochrane Review concluded that body weight support treadmill training improved walking velocity and endurance in individuals post-stroke who were independent ambulators9.
Currently, body weight supported treadmill training lacks statistically significant effect in the randomized controlled trial research literature due to the variability of client populations and treatments used with body weight supported treadmill training. However, prospective observational cohort studies are reporting statistically significant effects and body weight supported treadmill training is supported by neurophysiological evidence.
Research is still needed to define:
- Patient selection criteria and goals for body weight supported treadmill training
- Optimal speeds, duration of treatments, de-weighting amounts, and facilitation used during body weight supported treadmill training
Appropriate Body Weight Loading during BWSTT
In order to optimize the results of BWSTT, we need to know how much of the client’s weight should be supported by the harness. Although there has been no evidence for the ideal de-weighting, it has been shown that less than 30% of body weight support results in the most typical gait pattern, which is what we are aiming for with this type of treatment.
It is widely accepted that limb loading (i.e. weight-bearing through the legs) plays a role in modulating CPG activity and influencing supraspinal structures.Thus, we need to ensure that an appropriate amount of weight is being transferred through the client’s legs during BWSTT, so that the neurological systems are getting the full benefits of this training.
One of our primary systems involved in movement, called anticipatory postural adjustments (APA’s), have shown changes associated not only with mechanical aspects of a task but also with its perceptual aspects (i.e. fear of falling). By using the BWSTT there is an increased feeling of safety and decreased fear of falling, which allows for appropriate responses by the APA’s.

Using BSWTT to Increase Walking Speed
In addition to de-weighting and providing support to the client, using the BWSTT allows therapists to manually facilitate the client (hands-on assistance) at the feet, knees, and hips. This manual assistance improves the client’s gait patterning and decreases compensatory strategies. Together, these factors allow a client to improve their stepping ability and increase their walking speed.
Strong relationships have been established between walking speed and motor recovery, lower limb strength, and maximal ankle power. In addition, fast walking improves symmetry in double and single-support proportions in persons post-stroke.
The Central Pattern Generator (CPG) is speed dependent and has been shown to be inactive when stepping at slow speeds. With increasing walking speed, the CPG is activated and the automaticity of the gait pattern improves.
In a study by Hedel, Tomatis & Muller in 2006, they found that increased walking speed led to the following:
- Increased cadence (steps/minute) & stride length
- Decreased variability (i.e. improved consistency of stepping)
- Swing phase & single stance duration increased
- Double stance decreased
- Increased amplitude of hip joint movement
- Significant differences in ankle movement
Overall, this means that by increasing the client’s walking speed, we can improve a number of factors that help in neurological recovery and functional independence. By using the BWSTT, increasing a client’s gait speed is possible and safe, even for client’s who have begun their neurological recovery.

Treatment Considerations
Although it seems that BWSTT is easy to apply to a wide variety of clients with neurological impairments, there are a number of factors that have a significant effect on the outcome of the BWSTT; and should be considered by the therapist before treatments. These factors include:
- Alignment and body posture / stability
- Upper limb (hand/arm) placement / dependence / role of light touch
- Use of de-weighting
- Footwear and Bracing
- Walking speed
- Manual Facilitation vs external assistance
- Intensity of the training
- Somatosensory information, vision, cutaneous input
- Previous training level of the client

BWSTT: More than just walking!
As with all physiotherapy treatments, the BWSTT needs to be tailored to a client’s specific functional goals and specific therapy treatment plan.
Because BWSTT provides improved safety and stability, it can allow clients to work on a wide variety of goals, such as stepping, balance exercises, and reaching tasks, and can result in numerous benefits.
Partial body weight support (PBWS) training is an evidence-based approach for walking training of children with neuromotor disorders (Novak et al., 2020) that uses task-specific strategies, intensive practice, with variability and active participation of the child, and result in functional motor skills.
PBWS consists of reducing the load on lower limbs through a suspension system, allowing upright posture and facilitating walking movements. The fundamental principle of this strategy is to reduce the demand for muscle strength to overcome the gravitational force during walking. Based on this concept, the partial support of the body weight can be performed by different equipment, ranging from the swimming pool to harness systems and robotic devices.
The swimming pool was the first weight support system used as early as 1500BC by Hindus and Egyptians. The first “out of the water” PBWS system was developed in the 1980s with the evaluation of the motor behaviour of cats with spinal cord injury (Alaimo et al., 1984; Lovely et al., 1986). That system consisted of a vest fixed to a rod that stabilized the cat’s trunk and forelimbs, while the hindquarters were stabilized by the tail, during the animal’s walk on a treadmill. The explanation for the cat still being able to walk on the treadmill, even with spinal cord injury, was that there were structures in the spinal cord, called Central Pattern Generators (CPGs), capable of producing cyclic and rhythmic movements, such as walking movements, independently of brain control. Currently, with the advancement of PBWS training studies in human, we know that not only the CPGs of the spinal cord but also brain structures related to motivation, anticipation and motor adjustments that justify the great results on walking skill of individuals with different neurological conditions, including cerebral palsy and Down syndrome.

APPLYING PBWS TRAINING
There are several ways of applying PBWS in therapy that vary according to the basic elements of suspension systems. These elements include the way the suspension is applied, the stabilization to maintain the ideal posture, the way the individual’s body is attached to the system, the type of support surface on which the training is carried out and the amount of assistance the child needs to walk.
PBWS systems
The main element of PBWS is the way the suspension force is applied to the child. The suspension system has the function of complementing the muscle strength necessary to overcome gravity and keep the child standing, and to reduce joint compression in the lower limb joints and trunk as well. The child feels safe in the execution of the task, which motivates them to walk.
The suspension can be performed by a harness attached to a fixed point or rail, a counterweight system, a Spider cage elastic cable system, a thrust in hydrotherapy or with a robotic walking trainer. There is no protocol for the amount of bodyweight allowed, but it is applied according to the skills and therapeutic goal of each child. The suspension is gradually reduced as the walking training progresses, allowing the child to develop strategies and take on the task by supporting his/her own body weight. As the suspension is gradually decreased, the child has the opportunity to develop greater postural alignment, coordination of movements and balance in a safe and efficient way.
The child can actively maintain the ideal posture for walking maintained by using his/her own balance strategies or resting his/her hands on the parallel bars or the support bars of the electric treadmill. For children who need more assistance to keep their posture straight and stable, parallel cables or lateral stabilizers can be added.
The connection between the child’s body and the suspension system is commonly performed by a vest or belt fixation. Wearing the vest or belt makes walking training safe as it minimizes the child’s need for completely efficient posture adjustments.
The child’s posture, movement and stability when on a PBWS system are influenced by two factors: the part of the body in which the vest or belt is applied, such as the pelvis, abdomen, torso or lower limbs, and the anchorage point, i.e. the place where the suspension cables are placed, which can be on a fixed or mobile point, such as a rail, at the ceiling.
The most appropriate PBWS set varies for each patient, and the choice should be made aiming at the point of balance between stability and freedom of movement, as well as safety and comfort.

Overground versus Treadmill PBWS training
PWBS training can be applied on the ground or the treadmill depending on the child’s ability and therapeutic goal. The use of the floor as a support surface has the advantages of generating greater cognitive stimulation by continually changing the visual field and by the high specificity of training. On the other hand, the treadmill offers a controlled environment, suitable for the control of walking speed, adequacy of joint positions, and does not require large spaces for execution. Furthermore, with treadmill training, some children can be motivated to self-improve based on values such as speed and distance travelled.

Therapist handling versus Robotic devices
The therapist’s handling, the movement of the electric treadmill or the robotic walking trainer can be used to assist in the execution of the motor components of each phase of the walking cycle. The therapist can apply handling to facilitate passive or active-assisted weight transfer between the lower limbs and to lift the foot off the ground to take the step, while the conveyor belt of the treadmill is useful to facilitate ankle and foot movements by “dragging” the foot backwards.
The device commercially known as Lokomat, or similar equipment, is a robot developed for treadmill training, which also perform passive or active-assisted steps, but without the need for support by therapists. The mobility of the robotic legs is synchronized with the speed of the treadmill. The robot seems to provide symmetrical trunk balance, coordination, propulsion and step change. There are indications to improve walking speed, cadence and single-leg support time during walking. Children can start robot training only from the age of four. However, research is still inconclusive on these benefits in children with neuromotor dysfunctions and researchers suggest that more studies should be conducted to indicate the effects of this new therapeutic strategy for that population (Ammann-Reiffer, 2017).

BENEFITS AND INDICATIONS OF PBWS TRAINING
Based on the principle of motor learning, task-specific training with lots of repetition and active participation of the child, like training under PBWS systems, promotes the best performance of the essential aspects of the walking skill, as motor control, muscle strength, fatigue resistance, cardiopulmonary conditioning, motivation and emotional safety (Booth et al., 2018).
Non-walking children can benefit from better trunk control and maintenance of sitting and standing position (Damiano and DeJong, 2009). For children who are able to walk, even for short distances, PBWS treadmill training can improve endurance, speed, stride length (Booth et al., 2018). Activities like sitting, get up from sitting, going up and down steps, long-distance courses, standing without hand support, which influences the independent mobility in the day to day of the child and the caregiver, also may be improved (Emara et al., 2016).
Children with Down syndrome also benefit from this strategy to accelerate their development of independent walking (Wu et al., 2008).
Rare and minor adverse events can be related to PBWS treadmill training, such as leg discomfort off the treadmill, which resolve without intervention; and development of blisters on the feet if the socks, shoes or orthoses are not properly placed during the training (Booth et al., 2018). The hip dislocation has not been reported as an adverse event for this therapeutic strategy (Meyer-Heim et al., 2007), which is a good point to consider in a patient group that is at risk for hip subluxation or dislocation.
It is important to remember that PBWS training is only one of the physiotherapy strategies for walking acquisition and improvement of children with neuromotor dysfunctions. There are some points to consider before proceeding with PBWS training, such as core stability, postural control, joint range of movement and muscle strength in the lower limbs, coordination and balance. For this reason, each child must have their therapeutic plan individually designed.


Product Tags and Keywords :
Un Weight Mobility Trainer ,Partial Body Weight Support System ,Gait Training System ,Biotronix Un Weight Mobility Trainer ,Partial Body Weight Support System ,buy un weight mobility trainer ,Premium quality Un Weight Mobility Trainer ,Un-Weigh Mobility Trainer OCU01, Un-Weigh Mobility Trainer OCU01(MS), Unweighing System With/Without Treadmill